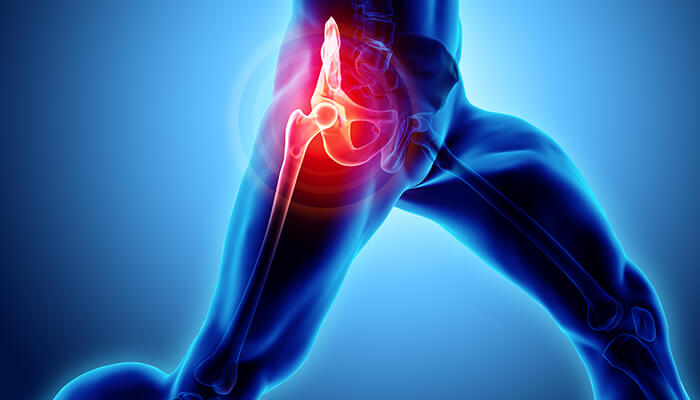
ESWT for Conditions of the Hip
ESWT Hip
Trochanteric Bursitis
Extracorporeal Shock Wave Therapy, or ESWT, was first developed 20 years ago as a treatment for kidney stones. Now researchers have found this treatment effective in treating a wide variety of joint conditions. Specifically, ESWT is now proving itself effective in several common conditions of the hip which have typically been resistant to non-invasive treatment. When physical therapy, NSAIDS, or rest and ice fail to alleviate hip symptoms, doctors have typically used surgery as the next option. However, with ESWT, treatment is applied in only one session, in the doctor’s office, lasting only twenty minutes. Both trochanteric bursitis of the hip and avascular necrosis of the hip (femoral head) are routinely treated with Shockwave Therapy.

Bursitis is a painful condition caused by chronic inflammation of small, fluid filled protective sacs found around joints. When this occurs to the bursa protecting the large, bony prominence on the outside of the femur just below the hip bones (the greater trochanter), it’s called trochanteric bursitis. It’s both extremely common and can be quite painful. Frequently, it’s known simply as hip bursitis. This condition typically starts off with only mild pain, and like many chronic joint conditions tends to get worse over time.
Signs and symptoms that your hip pain may be trochanteric bursitis:
- The classic symptom is pain and tenderness just below the greater trochanter
- Typically, no pain is felt inside the hip joint itself
- Pain radiating from the greater trochanter down the side of the hip
- Worse with running and walking
- Visible swelling and redness may or may not be present
Is surgery ever necessary for trochanteric bursitis?
In most cases, surgery is not necessary for trochanteric bursitis. Trochanteric bursitis can often be effectively treated with conservative measures, such as rest, activity modification, physical therapy, and medications. However, in some rare and severe cases where conservative treatments fail to provide relief, surgery may be considered as an option.
Surgical intervention for trochanteric bursitis is typically reserved for individuals who experience chronic, persistent pain that significantly impacts their daily activities and quality of life. Surgery aims to remove or repair the inflamed bursa and address any underlying structural issues contributing to the condition.
There are different surgical approaches that can be considered, such as bursectomy (removal of the bursa), tendon release or lengthening, or addressing any anatomical abnormalities. The specific procedure will depend on the individual’s case and the underlying factors contributing to the trochanteric bursitis.
It is important to note that surgery is usually considered as a last resort after exhausting non-surgical treatment options. The decision to undergo surgery should be made in consultation with a healthcare professional who can evaluate the severity of the condition, assess the potential benefits and risks of surgery, and provide personalized recommendations based on the individual’s specific circumstances.
It is always recommended to explore conservative treatments first and give them sufficient time to work before considering surgery for trochanteric bursitis.
Are there any complications associated with trochanteric bursitis?
While trochanteric bursitis itself is not typically associated with severe complications, if left untreated or if the underlying causes are not addressed, it can lead to chronic pain and functional limitations. Additionally, over time, compensation mechanisms due to pain and altered movement patterns may contribute to the development of secondary issues such as muscle imbalances, hip joint problems, or gait abnormalities. Early intervention and appropriate treatment can help prevent complications.
Avascular Necrosis
Avascular necrosis (AVN) of the hip joint is a less common but potentially much more severe condition. Any bone, including the femur, is living tissue which requires a surprisingly high level of circulation to remain healthy. Whenever this blood flow is lessened, the bone itself can begin to die. This is known as avascular necrosis.
Therapy Alternatives
There are numerous treatment options, with complete hip replacement being the most popular (THR). THRs can have certain drawbacks, too, like extended recovery times and shortened hip joint lifespans. In the elderly population, THRs are an useful kind of treatment; but, in younger individuals, they may lose their effectiveness before the end of a person’s life.
Depending on how much damage has been done to the femoral head, other treatments such metal on metal resurfacing might not be appropriate in all instances of avascular necrosis.
Bisphosphonates that slow down bone deterioration may stop collapse (particularly of the hip) brought on by AVN.
Compression of the core
Other treatments include free vascular fibular graft (FVFG), in which a piece of the fibula is removed along with its blood supply and implanted into the femoral head, and core decompression, in which internal bone pressure is relieved by drilling a hole into the bone and a living bone chip and an electrical device to stimulate new vascular growth are implanted. According to a Cochrane review, there is no discernible difference in outcomes between patients who undergo hip core decompression and physical therapy and those who receive only physical therapy. Furthermore, there is little solid information on the benefits of hip core decompression for sickle cell disease sufferers.
Transplanting nucleated cells from bone marrow into avascular necrosis lesions following core decompression may be able to stop the disease from progressing, but much more research is required to confirm this method.
Additional Causes
Bone fractures, joint dislocations, alcoholism, and the use of high-dose steroids are the main risk factors. Radiation therapy, chemotherapy, and organ transplantation are further risk factors. Cancer, lupus, sickle cell illness, HIV infection, Gaucher’s disease, and Caisson disease are all linked to osteonecrosis (dysbaric osteonecrosis). The disease could also develop for no apparent reason.
Signs and symptoms that your hip pain may be avascular necrosis: Note that in its early stages, avascular necrosis may be painless
- Pain is typically felt inside the hip joint itself
- Initial stages often present as pain when putting weight on the bone (standing)
- Pain is almost always worse when walking, jogging, or running
- A clicking or “ratcheting” may be felt, especially in later stages
- Note that the pain of AVN sometimes mimics the pain of other hip conditions.
Hip Extracorporeal Shockwave Therapy FAQs:
What is avascular necrosis (AVN)?
Avascular necrosis occurs when normally healthy tissue begins to die due to a lack of blood flow. The word “vascular” refers to blood vessels and blood circulation. The word “necrosis” means cell or tissue death. Avascular necrosis can occur anywhere in the body, but is found most often in bones with a poor blood supply. Specifically, our New York hip ESWT avascular necrosis patients usually present with AVN of the femoral head inside the hip socket. Avascular necrosis is always a serious condition requiring medical attention.
What causes avascular necrosis?
Most patients don’t realize that bone is living tissue with a rich blood supply. Any time that the blood supply to a bone is decreased, avascular necrosis can occur. AVN often occurs without an obvious cause, and many of our ESWT hip avascular necrosis New York patients have a history of the following:
- Long term corticosteroid use (cortisone). Taken either orally or injected, cortisone use is associated with over 35% of all avascular necrosis cases.
- Sickle cell disease
- HIV infection
- Chemotherapy and radiation therapy for cancer
- Longstanding degenerative arthritis
- A history of traumatic injury of the hip joint or pelvis
What are the signs and symptoms of avascular necrosis?
At first, there may be no symptoms at all. Many of our avascular necrosis talus Pittsburgh patients only learn they have AN during routine X-rays, sometimes in preparation for a hip replacement. The first symptoms usually felt are a usually sharp hip pain, directly inside the joint, which typically becomes more constant as the disease progresses. Eventually the joint can be affected to the point where the bone collapses—resulting in severe pain whenever the joint is used. As an extremely general rule, the time elapsed between the first feelings of pain and bone collapse ranges from 6 months to over a year.
What Are Risk Factors Of Avascular Necrosis?
There are many causes of Avascular necrosis but there are some risk factors that can increase the chances of you developing this problem even more.
Here are some of those risk factors:
- Drinking Too Much Alcohol
Fatty deposits can form in blood vessels if you drink too often, and if then drink several times a day then you are putting yourself at a huge risk.
Which means being a heavy drinker can badly affect your health and increases chances of Avascular necrosis.
- Some Types Of Medical Treatments
There are some types of medical treatments that damage your organs, they may increase your risk too.
For example, organ transplants such as kidney transplant or radiation therapy for cancer can weaken your blood vessels and cause avascular necrosis.
- Injuries
Injury to adjacent blood arteries, such as a hip dislocation or fracture, can limit blood supply to the bones.
Prevention
To lower the risk of avascular necrosis and enhance overall health, do the following steps:
Alcohol Should Be Consumed In Moderation: One of the leading causes of avascular necrosis is excessive drinking.
Maintain A Healthy Cholesterol Level: The most prevalent material obstructing blood circulation to bones is teeny-tiny particles of fat.
Keep An Eye On Your Steroid Usage: Make sure your doctor is aware of any history or current usage of high-dose steroids. Repeated rounds of high-dose steroids appear to exacerbate steroid-related bone deterioration.
Please Don’t Smoke: Smoking constricts blood arteries, reducing blood flow.
Why does AVN commonly occur at the hip?
AVN can occur in any bone. However, bones which naturally have a poor blood supply are more vulnerable. The head of the femur (the “ball” part of the ball-and-socket joint) has a single small artery providing its entire blood supply, and many cases of AVN are seen here. Often our Cranberry ESWT hip avascular necrosis patients considering hip replacement surgery have an extensive history of arthritis in the hip joint. When enough degeneration occurs, blood supply can become affected.
What other bones are frequent sites for avascular necrosis?
In our Erie ESWT hip avascular necrosis patients alone, we’ve also seen AVN in the small bones of the wrist (typically the scaphoid), ankle, (typically the talus), mandible, and the area of the shoulder blade just to the inside of the shoulder joint. All of these bones or areas of bone have a poor blood supply.
What is trochanteric bursitis?
Bursa are small fluid filled sacs which protect joints. When they become chronically inflamed, it’s known as bursitis, much as chronic inflammation of tendons is known as tendonitis. The large bony “bump” on the side of hip just below the actual hip bones is known as the greater trochanter. When the large bursa pads which protect this part of the joint become inflamed it’s known as trochanteric bursitis. Many of our ESWT hip avascular necrosis Trenton area patients who come in with other hip problems present with bursitis as well.
What causes trochanteric bursitis?
This type of bursitis is typically an overuse injury, and it occurs with great frequency in runners. Years of walking and running contribute to almost all cases—especially if patients also have a large Leg Length Inequality (LLI). If the legs are of significantly different lengths uneven wear and tear results and can result in bursitis. Many of our New York ESWT bursitis patients also have a history of previous hip surgery. Often trochanteric bursitis doesn’t have an obvious cause.
What are the signs and symptoms of trochanteric bursitis?
Not surprisingly, the tell-tale symptom is almost always pain just below the greater trochanter. Very few of our Pittsburgh ESWT bursitis patients come in with pain in the actual joint. Although this is a chronic irritation and inflammation based condition, visible swelling isn’t always present. Pain starts out mild and becomes more severe as the condition progresses, and is almost guaranteed to be more severe when walking or running.
What are some common treatments for these conditions?
Only a few procedures are used to treat AVN. All are invasive, and complete joint replacement is considered a major surgery—invasive orthopedic procedures should always be a last resort.
Bone grafts:
As much as is possible, the damaged bone is removed in a procedure known as debridement. Healthy bone is harvested from another area of the body and implanted on the femoral head. Note that this isn’t always successful as this part of the hip joint generally has a poor blood supply to begin with. Although less invasive than a complete replacement, this is still a major surgery.
Total joint replacement:
This option is reserved only for severely damaged joints. Much as it sounds, the joint is removed and a artificial replacement is set into the hip socket and shaft of the femur.
A note on trochanteric bursitis:
Although the pain of bursitis can become severe, surgery is almost never an option. Treatment is typically limited to over the counter pain medications (NSAIDS), cortisone injections, and physical therapy. Often patients find themselves in a situation where their symptoms are severe enough to limit their daily activities, yet they find little relief with these conservative therapies. Unfortunately, bursitis of the hip is generally regarded as being resistant to treatment.
How can ESWT (Extracorporeal Shockwave Therapy) treat these conditions?
Extracorporeal Shockwave Therapy (ESWT) is an excellent treatment for avascular necrosis—it’s unique, in fact. Remember that avascular necrosis is bone death due to lack of blood circulation. To date, Shockwave Therapy is the only treatment recognized to cause an effect called neo-vascularization (the formation of many new capillary arteries in the area). ESWT effectively uses high-intensity ultrasound energy to “jump-start” the healing process. We feel that several of our Pittsburgh ESWT hip avascular necrosis patients have been saved from surgery thanks to Shockwave therapy.
Many chronic overuse conditions such as bursitis have two things in common—chronic inflammation and incomplete healing. Shockwave Therapy addresses both of these issues as described above.
Treatment with ESWT
During the session, you comfortably recline while the affected hip is placed on a warm water bubble and covered with gel. The injured area is viewed with diagnostic ultrasound. Then, we then deliver tiny little pressure waves or “shockwaves” to the injured area. Healing occurs gradually over the next 6-12 weeks.
Approved by the National Institute for Clinical Excellence for use on tennis elbow one year ago, we are happy to make this treatment available to you. Call our office today to begin experiencing the relief this treatment offers in one short session.
Sound Medical Technologies, Inc. offers several ESWT– related services. We provide trained staff and certified technicians to operate the equipment during ESWT procedures. Physician certifications, recommendations and our clinical applications specialist can answer all your questions.
Call Sound Medical Technologies to learn how you can have this technology available on a case-by-case basis, without purchase or lease. We deliver and set up the machine and provide you with educational materials for patients. Assist you in providing the procedure. You maintain control of the patient relationship. You receive the reimbursement into your practice.
